An amputee cannot generate a muscular force to cause the prosthetic joint to rotate other joints. Most frequently, the player’s hips must work significantly harder to enable the motion of a golf swing. For instance, a lower-limb amputee will not be able to push the leg from the ankle; instead, they will pull the leg from the hip. This change in harnessing ‘Ground Reaction Force’ can influence impact factors and subsequent ball flight patterns. Be aware of the positioning of the amputation, above or below the knee and above or below the elbow, as this can significantly influence mobility and elicit changes in movement patterns for golf.
Treating stump and phantom limb pain
Stump and phantom limb pain will usually improve over time, but treatments are available to help relieve the symptoms.
Medicines – Medicines that may be used to help relieve pain include:
- non-steroidal anti-inflammatory drugs (NSAIDs), such as ibuprofen, anticonvulsants such as pregabalin or gabapentin,
- antidepressants such as amitriptyline, or nortriptyline, which are useful in treating nerve pain -opioids such as codeine or morphine, corticosteroid or local anaesthetic injections.
Self-help measures and complementary therapy
There are several non-invasive techniques that may help relieve pain in some people. They include:
Mental imagery
Research has shown that people who imagine using the part of their limb that was amputated experience a reduction in pain symptoms. This may be related to the central theory of phantom limb pain. Researchers think the brain looks to receive feedback from an amputated limb, and these mental exercises may provide an effective substitute for this missing feedback.
Another technique, known as mirror visual feedback, involves using a mirror to create a reflection of the other limb. Some people find that exercising and moving their other limb can help relieve phantom pain.
Prosthetic limbs are not suitable for everyone who’s had an amputation because an extensive course of physiotherapy and rehabilitation is required. Adjusting to life with a prosthetic limb takes a considerable amount of energy because of having to compensate for the loss of muscle and bone in the amputated limb. This is why frail people or those with a serious health condition, such as heart disease, may not be suitable for a prosthetic limb.
Description – A prosthesis is an artificial device used to replace all or part of a missing limb. Prostheses are often used by someone who has experienced limb loss due to injury, accident, or illness, but they can also be used by someone with a congenital condition that results in a limb difference.
Unlike knee or hip replacements (“endoprostheses”), which are implanted in the patient’s limb, prostheses are worn by the user by attaching it to their residual limb. While not everyone with a limb difference or limb loss needs a prosthesis, the right device can empower users in many different ways. Keep reading to learn more about how.
The basic purpose of a prosthetic device is to restore the functionality and mobility of a missing limb, making it easier to take part in daily activities, hobbies, work tasks, and more. Prostheses can also improve users’ quality of life, empowering them to be as active as they want and are able to be – whether that means moving safely around their house or being a high-performance athlete. For people who have experienced a limb loss, a prosthetic device can also help reduce the emotional impact of an accident or injury.
There are many types of prostheses, from simple devices like mechanical or body powered devices to complex, high-tech ones that mimic the movement and functionality of a natural limb.
If an individual is able to have a prosthetic limb, the type of limb that’s recommended for will depend on:
- the type of amputation
- the amount of muscle strength in the remaining section of the limb
- general health
- tasks the prosthetic limb will be expected to perform
- whether the individual wants the limb to look as real as possible or is more concerned with function (golf specific)
If it’s thought that an individual would find it difficult to withstand the strain of using a prosthetic limb, a cosmetic limb may be recommended. This is a limb that looks like a real limb, but it cannot be used like a prosthetic limb.
It’s possible to have a prosthetic limb that’s both physically realistic and functional, but there may have to be an element of compromise between the different types.



Further information on types of prothesis are available via EDGA partner – Ottobock – click on the image below:
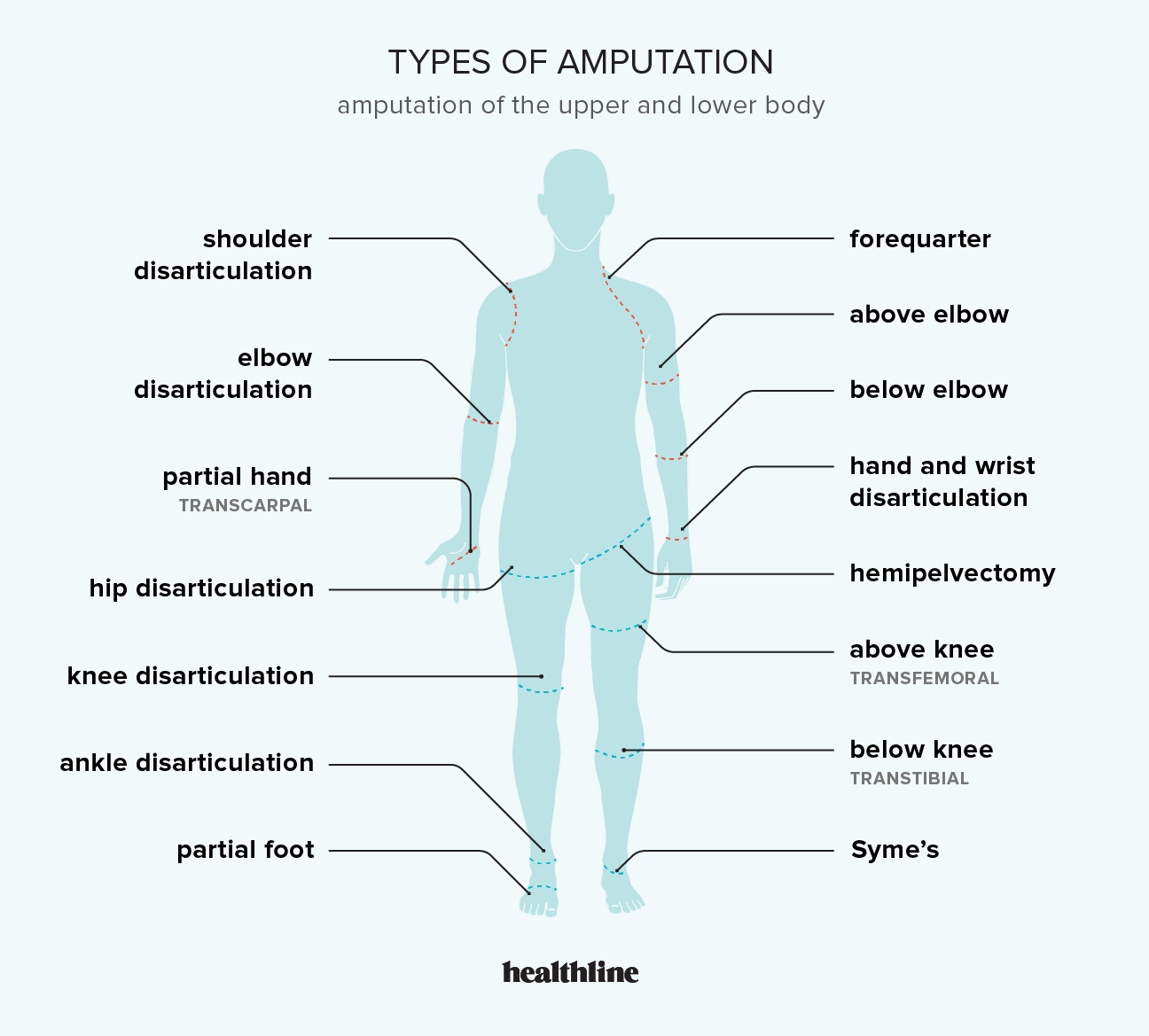
Levels of amputation
Mobility, range of movement, coordination, balance, and comfort vary greatly depending on the level of amputation. Generally, the more residual limb (stump length) an amputee has, the more mobile they will be.
Some common sites for amputation are:
- Partial foot or toe(s)
- Syme’s (through the ankle)
- Trans-tibial amputation (below the knee)
- Knee disarticulation (through the knee)
- Transfemoral amputation (above the knee)
- Hip disarticulation or hemipelvectomy
- Bilateral lower-limb loss
- Partial hand or finger(s)
- Wrist disarticulation
- Below elbow
- Elbow disarticulation
- Above elbow
- Shoulder disarticulation or fore-quarter
- Bilateral upper-limb loss
- Multiple amputations.
General characteristics
- Mobility, range of movement, coordination, balance and comfort vary greatly depending on the level and cause of the amputation/limb difference and individual player’s may have a preference to play with or without their prothesis on.
- Residual limbs (stump) can vary in quality (integrity) and length which may affect involvement and movement and would require specialised equipment – most golf club manufacturers are now more than competent in fitting players with bespoke equipment for limb differences.
- Congenital amputees may have less stump pain, discomfort and soreness than those who have lost limbs through injury which may Impact on the length of time a player can
play or train for. - Be mindful of fatigue in the arms and upper body, as well as blistering on the hands when using crutches. Sports gloves, blister plasters and additional padding on the
crutches (if used)can help mitigate the risk of developing blisters.

- Amputee players have greater difficulty regulating body temperature because the ratio of surface area to body volume is different and could result in overheating. Coaches
must therefore ensure players wear suitable clothing and ample opportunities are provided for rehydration, rest and recovery. - Perspiration and volume change during activity can affect the prosthetic fit and comfort. Players may need time to adjust their socket during play, so time and an appropriate location need to be provided for this.
Sockets & Liners
What is socket technology?
A prosthetic socket is a crucial component in a prosthesis. It acts as the interface between the prosthetic technology and the residual limb. If it doesn’t fit correctly, amputees can experience pain, sores and blisters, and the prosthesis will feel heavy and cumbersome. As a result, an amputees ability to move freely without pain may be compromised and they may not use their prosthesis at all. To help avoid this discomfort, various different methods of securing the prosthesis to the residual limb exist.
Maintaining a healthy residual limb can be challenging and a contributing factor to the overall comfort of the socket. To support this, a variety of prosthetics liners are available, each offering a range of specific benefits to suit the amputee’s individual circumstances.
More detailed information on the various types of sockets and liners can be found via clicking on the image below




Motion Pattern Examples
Note the differences in swing direction and energy loading in the following videos. Note the changes in videos of players playing with various limb differences and amputation.
Trail Arm player – with prothesis
Player Stories
Gain further insights to how golfers with limb difference and amputation play via the ‘EDGA Player Stories’ – Click on the following images to read and listen to a selection of interviews.










Further ‘Player Stories’ can be found via clicking on the image link below:

*This material remains the intellectual property of the EDGA Educational team and may not be distributed or used further without written consent from the EDGA Educational team.
